Inherited arrhythmias, such as Long QT syndromes (LQTS), are one of the most common causes of cardiovascular disease-related death among young people. LQTS is characterized by delayed ventricular repolarization, which predisposes patients to suffer ventricular arrhythmias and sudden death. LQTS type 2 is caused by mutations in the hERG potassium ion channel coded by the KCNH2 gene. Environmental factors and the presence of additional common genetic variants can alter the disease expressivity, which complicates the stratification and clinical management of patients.
The common single nucleotide polymorphism (SNP) KCNH2-K897T can potentially act as a genetic modifier of LQTS2. However, establishing its exact contribution to the disease-phenotype has been challenging. Studies with human cohorts and families have led to contradictory results, classifying KCNH2-K897T either as protective or exacerbating of the LQTS2 phenotype.
To unravel the functional impact of the SNP KCNH2-K897T in patients with LQTS2, van den Brink, L., et al. [1] used isogenic human induced pluripotent stem cell (iPSC)-derived cardiomyocytes with a LQTS2-causing mutation, combined with the SNP KCNH2-K897T potential modifier in two different positions: same allele (cis) or opposite allele (trans).
Key takeaways
-
Functional comparisons between the two human iPSC-based models indicated that the line carrying SNP KCNH2-K897T in cis exacerbated the phenotype of LQTS2 (Fig. 1). This line showed longer action and field potential durations and increased arrhythmogenic response to the hERG channel blocker E4031.
-
Use of isogenic human iPSC lines is critical to understand the influence of genetic-modifying variants because it avoids the intervention of background-related variability that might lead to contradictory clinical outcomes.
-
This study demonstrates that disease models based on human iPSC-derived cardiomyocytes are facilitating investigations into the functional impact of genetic modifiers for inherited arrhythmias.
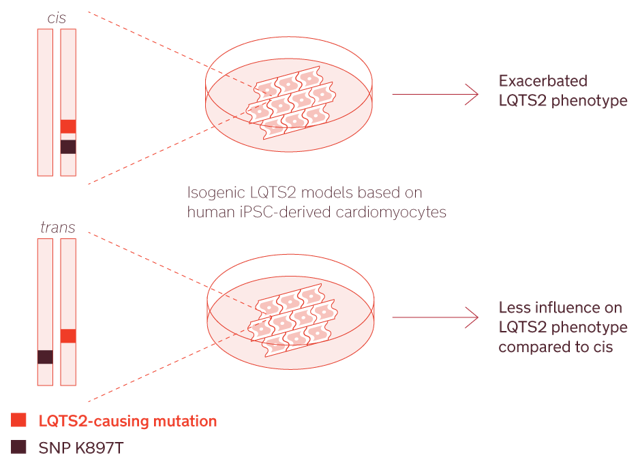
Figure 1. Modeling LQTS2 with human-iPSC cardiomyocytes to study the effect of genetic modifiers.
Reference
[1] van den Brink, L., Brandão, K. O., Yiangou, L., Blanch-Asensio, A., Mol, M. P., Mummery, C. L., Verkerk, A. O. & Davis, R. P. (2021). The Linkage Phase of the Polymorphism KCNH2-K897T Influences the Electrophysiological Phenotype in hiPSC Models of LQT2. Frontiers in physiology, 2177. https://doi.org/10.3389/fphys.2021.755642
